Astonishing discovery in Manchester offers new lease of life for leukaemia-stricken children
- Written by Thom Bamford
- Last updated 1 year ago
- Community, People

Manchester’s Groundbreaking Leukaemia Study
This groundbreaking study has demonstrated remarkable results, offering a potential lifeline to patients who had previously exhausted all treatment options.
The innovative treatment owes its success to newborn babies, as cord blood cells extracted from the placenta, coupled with white blood cell transfusions, have proven to be the most effective therapy ever trialled.
Meet Sarah, an eight-year-old girl from Cornwall who was diagnosed with acute myeloid leukaemia (AML) at the tender age of four.
AML is a rare form of childhood leukaemia, affecting approximately 100 children and young adults in the UK annually. Despite undergoing various treatments, including chemotherapy and a bone marrow transplant, Sarah’s condition did not improve.
Royal Manchester Children’s Hospital
Consequently, she travelled to Royal Manchester Children’s Hospital (RMCH), part of Manchester NHS Foundation Trust (MFT), to participate in the GRANS clinical trial, hoping for a miracle. Now, over a year in remission, Sarah’s family and the RMCH team are optimistic that this groundbreaking treatment has potentially cured her leukaemia.
Sarah was among ten children involved in the two-year study who received cord blood stem cell transplants combined with a series of white blood cell transfusions, known as granulocytes, aimed at enhancing the cancer-fighting capabilities of the new cord blood.
A cure for leukaemia
Sarah’s mother, Simona Marica, a 44-year-old staff nurse, shared her emotional journey: “When I heard the doctor diagnose Sarah with leukaemia, I started crying at the word. But what was even worse was the news that this was a rare, more difficult-to-treat form of leukaemia. Her condition was so severe that she had to start chemotherapy immediately, as her blood results were critically bad, and she could have passed away at any moment.”
Simona continued, “After undergoing six months of chemotherapy in Bristol, she achieved remission, and we were regaining a sense of normalcy in our lives. That was in 2019, but in February 2020, the leukaemia returned. She had more chemotherapy, and fortunately, our ten-year-old son David was a bone marrow match and donated it to Sarah, who then underwent a stem cell transplant and achieved another 18 months of remission.”

It was during Sarah’s third chemotherapy treatment that doctors in Bristol discussed the possibility of her participating in the GRANS study at RMCH.
Simona shared her thoughts, saying, “I knew that a second transplant would be her last chance. Being a nurse, I was aware that if the leukaemia returned again, there would be no further treatment options available. Sarah’s body wouldn’t be able to withstand any more chemotherapy or other treatments. I knew this trial was her last chance of life.”
The British Journal of Haematology
The initial findings from the study have been published in the British Journal of Haematology, and based on the promising results, the trial has been expanded to include more patients from across the UK. Researchers are also delving into the scientific aspects of this treatment to gain a deeper understanding of its mechanisms and efficacy.
Professor Rob Wynn, Consultant Paediatric Haematologist and Director of the Paediatric Bone Marrow Transplant Programme at RMCH, expressed his thoughts on the research: “Our previous research, as reported in the Blood Advances journal, indicated that cord blood cells offer the most effective treatment for children with challenging blood cancers. The GRANS clinical trial builds upon this knowledge and provides a treatment option for the most critically ill children with AML, who previously had no available treatments.”
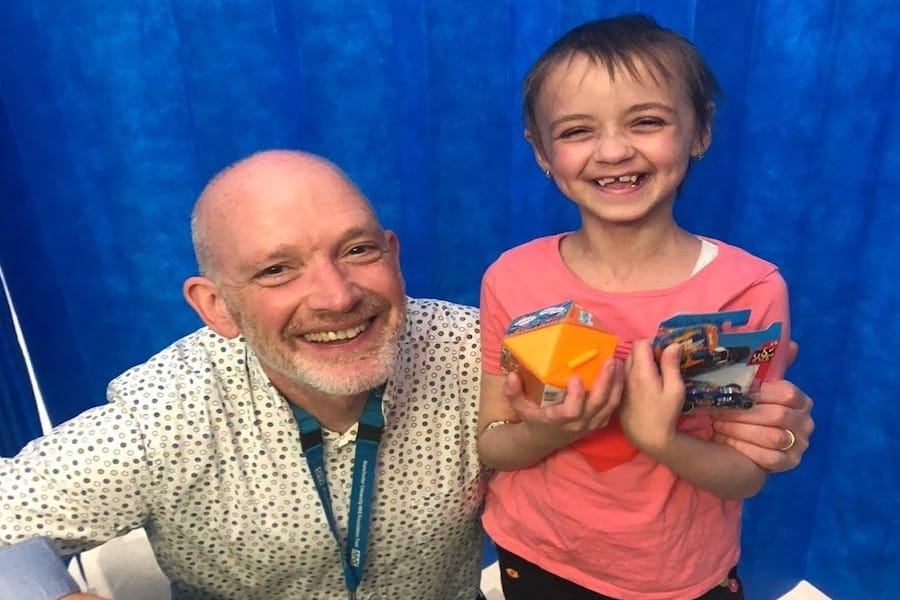
Professor Wynn further added, “Sarah is one of five children from our trial who are alive and in remission due to this effective experimental treatment. Without this clinical trial, it is highly unlikely that any of these children would still be alive. As a leading transplant center, we have the expertise to conduct this specialised and transformative research for children across England, and we are committed to sharing these remarkable results.”
With Sarah now surpassing one year in remission, her family can finally leave behind the pain of the past few years and focus on the future. This summer, they eagerly anticipate a holiday in France with friends and the chance to experience a normal family life once again.
Simona expressed her gratitude, saying, “I am incredibly grateful that Sarah was able to participate in the trial. Professor Wynn and the entire team made us feel like family, taking exceptional care of us throughout the process. They are truly doing amazing things. Sarah has been through so much over the past few years, but she has shown immense bravery. She has been my rock, a cheerful and determined girl who loves school and playing with her friends. Thanks to this research, Sarah is now fully enjoying life. She is my inspiration, and this treatment has given us our lives back.”
Understanding the Treatment: The Science Behind It
Granulocytes have historically been administered to patients with severe infections at the time of transplant to bolster the body’s ability to combat infection. Researchers at RMCH, however, noticed that when granulocyte transfusions were administered shortly after a cord blood transplant, the immune cells, known as T-cells, from the cord blood recovered much more rapidly. Notably, T-cells are recognised as the most potent fighters against leukaemia cells.
In the GRANS study, the children received seven granulocyte transfusions around the time of their transplant. Interestingly, these transfusions were administered even if the patients did not have serious infections. The goal was to deliberately increase the number of cord blood T-cells, thereby enhancing the immune system’s recovery. Researchers closely examined the impact of white blood cell transfusions on the immune system recovery of the newly transplanted cord blood.
In conjunction with the clinical trial, laboratory investigations supported by The Little Princess Trust were conducted, with grant management and expert assistance from the Children’s Cancer and Leukaemia Group (CCLG). These investigations aimed to unravel the properties of cord blood T-cells, their response to granulocytes, and their potential for eradicating leukaemia.
Phil Brace, Chief Executive of The Little Princess Trust, highlighted the importance of this research: “As one of the UK’s largest charity funders of childhood cancer research, we are dedicated to supporting research and trials that enhance patient outcomes. The remarkable progress made by Professor Wynn and his team in Manchester, along with the incredible bravery demonstrated by Sarah and her family, inspire us all to continue focusing our efforts on funding scientific endeavors that will lead to kinder and more effective treatments for childhood cancers. We are tremendously grateful to our supporters, as their contributions ensure we can fund clinical trials. Witnessing research funded by The Little Princess Trust deliver such incredible results fills us with pride.”
Exploring Cord Blood Transplants to Cure AML
Cord blood, which remains in the placenta and umbilical cord after childbirth, is a rich source of stem cells and represents a potential treatment option for children with AML when chemotherapy fails.
Cord blood transplants are only considered when all other treatment alternatives have been exhausted due to associated risks, including graft-versus-host disease (GVHD). GVHD occurs when the donor’s immune cells attack the recipient’s healthy cells and can lead to severe complications, including life-threatening situations.
Research conducted by the RMCH team revealed that children receiving cord blood transplants after unsuccessful chemotherapy were nearly five times more likely to be disease-free and GVHD-free compared to those who received other stem cell transplant options.
Professor Wynn emphasised, “In Manchester, we have been strong advocates for using cord blood due to our research demonstrating that this type of transplant yields the best outcomes for our patients.
“However, the number of cord blood transplants in the UK has been declining. In comparison to bone marrow transplants, cord blood transplants are more challenging and result in prolonged hospitalisation and significant illness in children. Consequently, children are often referred to us from hospitals across the country. Our next steps involve further research to better comprehend the immune effects of cord blood and granulocytes so that we can refine and optimise this treatment to cure children with difficult-to-treat leukaemia.”
Although the placenta and umbilical cord are typically discarded after birth, cord blood is collected and stored in dedicated facilities in the UK. NHS Blood and Transplant (NHSBT) and Anthony Nolan, a UK charity, closely collaborate in managing donor databases.
NHSBT’s skilled and specialised personnel collect cord blood donations at two hospitals in London and one in Luton. They also supplied the cord blood units for the transplants and the granulocytes, a blood product comprising white blood cells from ten donors pooled into a single product, utilised in the GRANS study.
Anthony Nolan oversees cord collection sites at Saint Mary’s Hospital on Oxford Road and Saint Mary’s at Wythenshawe, both of which are part of MFT. These sites enable parents to donate their baby’s placenta and umbilical cord to the charity for stem cell donation or research.
Henny Braund MBE, Chief Executive at Anthony Nolan, remarked, “Anthony Nolan’s cord blood program was established in 2008 to address the unmet needs of patients. This research provides crucial answers for children with limited treatment options, and we hope it paves the way for further research that will save more lives in the future.”
Guy Parkes, Head of Stem Cell Donation and Transplantation at NHS Blood and Transplant, expressed pride in supporting this significant research and acknowledged the vital role and benefits of cord blood and blood products as treatment options. He also highlighted their continued investment in maintaining the UK’s largest public cord blood bank.
This groundbreaking research conducted at the Royal Manchester Children’s Hospital not only offers hope to children with rare, high-risk leukaemia but also provides valuable insights into the potential of cord blood transplants and granulocyte transfusions.
As the trial expands to include more patients across the UK, the scientific community eagerly anticipates further discoveries that will improve outcomes and revolutionise treatments for childhood cancers.
- This article was last updated 1 year ago.
- It was first published on 3 July 2023 and is subject to be updated from time to time. Please refresh or return to see the latest version.
Did we miss something? Let us know: [email protected]
Want to be the first to receive all the latest news stories, what’s on and events from the heart of Manchester? Sign up here.
Manchester is a successful city, but many people suffer. I Love Manchester helps raise awareness and funds to help improve the lives and prospects of people across Greater Manchester – and we can’t do it without your help. So please support us with what you can so we can continue to spread the love. Thank you in advance!
Got a story worth sharing?
What’s the story? We are all ears when it comes to positive news and inspiring stories. You can send story ideas to [email protected]
An email you’ll love. Subscribe to our newsletter to get the latest news stories delivered direct to your inbox.

Review: Paraorchestra’s Symphony of Sorrowful Songs at RNCM is a ‘life affirming, joyously uplifting experience’

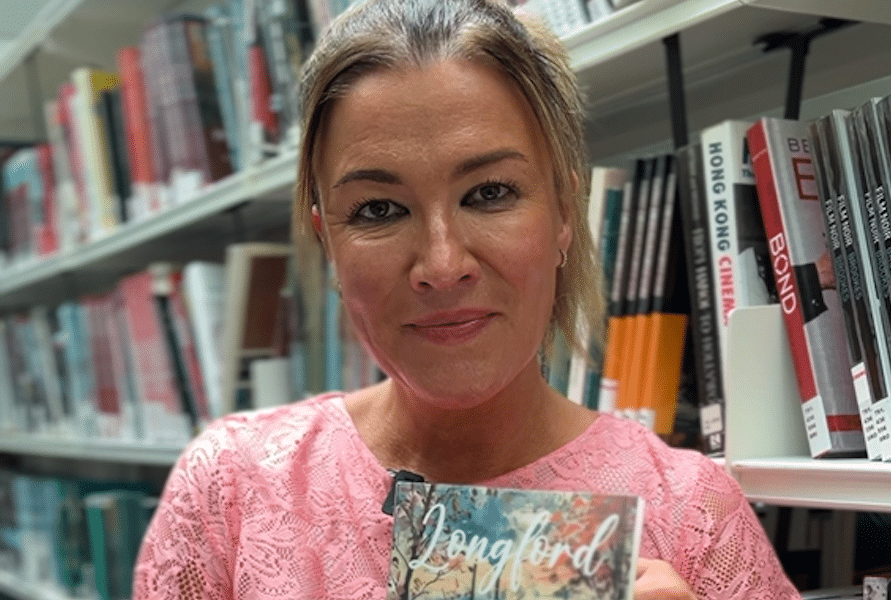
Author explores a love that helped build our city in her gorgeous debut novel

Inside the plan for 600 new ‘genuinely affordable’ and super energy-efficient homes in Manchester

The inspiring duo who sparked a 24-hour run to help Manchester’s homeless

“We want to ensure Manchester remains an inclusive cultural capital” Free to use artist hub will open in 2025