Manchester’s forgotten sufferers: living with dementia in the shadow of COVID-19
- Written by Joseph Timan
- Last updated 2 years ago
- Charity, People

The retired clinical scientist who had worked for the NHS became a carer for his wife, Teresa, after she was diagnosed with dementia in 2014 at the age of 66.
Since then, her symptoms had worsened and the situation had become more challenging. In the new year, the Seneviratne family decided it would be best for Teresa to live in a care home where she would receive the attention she needed while Jeff could visit regularly and spend more quality time with her.
Two days before the national lockdown began in March 2020, Teresa moved into a care home in south Manchester. The 71-year-old died 10 days later.
“It was a really terrible time,” Jeff recalls, speaking of the difficulty in arranging a funeral with the tight restrictions which were in place during the pandemic. The couple, who have lived in south Manchester since the seventies, had been through a lot together – but Jeff considers himself lucky compared to others.
Retiring around the same time Teresa was diagnosed with dementia, Jeff says his caring duties were still ‘light’ when he discovered that he had bowel cancer two years later. Having had the all clear now after undergoing surgery twice with some chemotherapy in between, Jeff says the care he received from the NHS while he had cancer is incomparable to his wife’s experience of dementia.
The couple – who founded the Didsbury Beer Festival – first spotted the signs of dementia some time before Teresa’s diagnosis. In 2012, she saw a doctor to discuss the memory problems she had, but the investigation was inconclusive.
Looking back now, Jeff says symptoms started presenting themselves several years earlier. But it was not all about memory – orientation was an issue for Teresa who would forget where she parked or struggle to find her hotel room.
Years later, Jeff would get phone calls from his wife when she missed a turning on the motorway and he would have to talk her through finding her way again. It was then that the couple decided Teresa was due another visit to the doctor.
Despite a diagnosis of dementia in October 2014, it wasn’t until the following summer that Teresa was told she had Alzheimer’s disease, the most common cause of dementia in the UK. “All this time we were in limbo,” Jeff recollects.
“Nobody followed up. We’d just been given some life-changing information.”
After this diagnosis in 2015, Teresa was prescribed medication – but that was it, according to Jeff. “Apart from the drugs,” he said, “there was no follow up.
“Everything you needed, you had to arrange to see the GP. We didn’t feel that we were in a system of care.”
The adventurous couple continued travelling for some years after Teresa’s diagnosis, including a trip to Norway in 2016 to see the Northern lights. But while on a trip to the Isle of Skye a year earlier, Jeff came to a realisation.
“I realised that if we’re going out into the mountains and the lakes, I’m effectively on my own now,” he explained, talking of the trip to Scotland.
Teresa maintained good relationships with her family throughout her illness, Jeff says, perhaps finding it hard to put a name to a face, but not forgetting it. However, towards the end of her life, even grandchildren as young as three knew they needed to look out for their grandmother who had hit her seventies.
Jeff recalls his grandchildren alerting him to Teresa lifting the lid of a pan on the stove or shouting, “granddad, grandma’s come out the door”. By this point, Teresa needed more help getting dressed and showered so Jeff employed the services of a care agency to help for around an hour in the morning every day.
A device which would alert Jeff when his wife got out of bed was installed, but only after he had sought a solution himself. “I had to ask the question,” he said.
“Nobody said, ‘this will be helpful’. Why did I have to ask for that?”
The problem with dementia, Jeff argues, is that it does not neatly fit into a medical model of care. The responsibility lies in both health and social care.
But neither the NHS nor local councils ‘own’ the responsibility, he claims, so patients and their families who care for them often fall between the cracks. In contrast, when Jeff was diagnosed with bowel cancer, there was ‘a whole system that clicked into place’, with appointments arranged immediately and the coordination between different parts of the NHS described as ‘seamless’.
“As soon as I was discovered to have bowel cancer,” Jeff said, “there was a specialist nurse who said, ‘here’s a card – ring us if you have any questions. This is what’s going to happen now…’”
Jeff is now the chair of trustees at Together Dementia Support, a Manchester charity which helps people with dementia live positively and supports carers. The organisation, which supports people in Trafford too, estimates that there are around 5,000 people across Manchester currently living with dementia.
Jeff first became associated with the charity when Teresa founded Fabulous Forgetful Friends, an ‘influencing group’ which also helps people living with dementia continue to enjoy life. He believes that third sector support groups like these need more recognition and more funding directed towards them.
The organisation he now chairs currently supports around 300 carers every week. On Wednesday (April 19), carers and former carers associated with the organisation met in Alexandra Park to share memories of their loved ones.
It was an emotional event. But for some, there is still a sense of frustration.
In March, Jeff told Manchester council’s health scrutiny committee of his story, concluding that there is ‘no system of care’ for dementia patients. He called for a system incorporating GPs, specialists, carers and charities to be created.
He praised the progress made at the town hall which published a report that recognises some of the changes needed. It builds on the work already under way with Greater Manchester Integrated Care’s Dementia United programme.
“If we do this in Manchester,” he told councillors at the public meeting on March 8, “we could become a model which others might want to replicate.”
- This article was last updated 2 years ago.
- It was first published on 27 April 2023 and is subject to be updated from time to time. Please refresh or return to see the latest version.
Did we miss something? Let us know: [email protected]
Want to be the first to receive all the latest news stories, what’s on and events from the heart of Manchester? Sign up here.
Manchester is a successful city, but many people suffer. I Love Manchester helps raise awareness and funds to help improve the lives and prospects of people across Greater Manchester – and we can’t do it without your help. So please support us with what you can so we can continue to spread the love. Thank you in advance!
An email you’ll love. Subscribe to our newsletter to get the latest news stories delivered direct to your inbox.
Got a story worth sharing?
What’s the story? We are all ears when it comes to positive news and inspiring stories. You can send story ideas to [email protected]
While we can’t guarantee to publish everything, we will always consider any enquiry or idea that promotes:
- Independent new openings
- Human interest
- Not-for-profit organisations
- Community Interest Companies (CiCs) and projects
- Charities and charitable initiatives
- Affordability and offers saving people over 20%
For anything else, don’t hesitate to get in touch with us about advertorials (from £350+VAT) and advertising opportunities: [email protected]


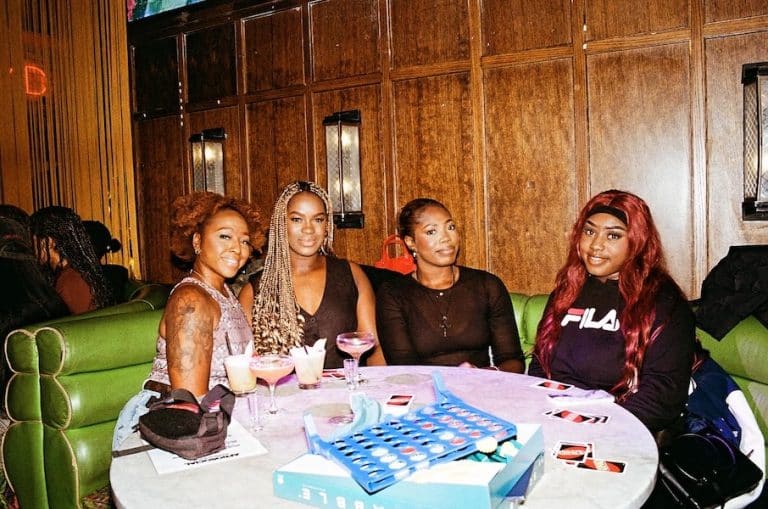
Afrosocial is changing the game for Afro-Caribbean professionals in Manchester


From paws to applause: Could your dog be Manchester’s next big opera star?